Australians playing sport or working in physical jobs for extended periods in hot weather or environments risk gut damage and blood poisoning that may lead to serious illness.


For the first time, a Monash University-led research project has identified the point at which people face potentially serious Exercise-Induced Gastrointestinal Syndrome (EIGS), and the corresponding degree of seriousness.
EIGS can cause a range of debilitating signs and symptoms, as a result of pathogenic agents (e.g. bacteria or bacterial endotoxins) in the gut leaking into blood circulation.
This situation may lead to more serious clinical implications such as sepsis, if the body’s immune system can’t cope with these pathogens in the blood. EIGS mimics similar health conditions such as ischaemic bowel disease, irritable bowel syndrome, and inflammatory bowel disease.
Published in Temperature, the study found that a rise in core body temperature to 39°C, and above, from two hours of exercise in hot conditions can predict the onset of gut damage and the movement of pathogens from the gut into the bloodstream, as part of EIGS.
As core body temperature increased, the extent of gut damage, bacterial endotoxin, systemic inflammatory responses, and gut symptoms also rose.
Lead author Kayla Henningsen, a Dietitian and Exercise Gastroenterology PhD candidate at Monash University’s Department of Nutrition, Dietetics and Food, said EIGS could occur during sports activities or even work.
“Physically demanding fields, such as the mining industry, military, agriculture and firefighting services, are notorious for not only the exertional activity required to fulfil the role of the occupation, but also for the potential of heat exposure,” Ms Henningsen said.
“Occupations that require high levels of physical labour while being exposed to extreme heat conditions could also experience gut symptoms from exertional-heat stress, leading to an increase in the risk of systemic shock, infections in the bloodstream, or even death if not treated appropriately.”
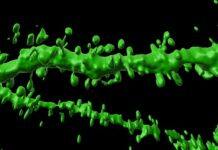
EIGS can occur when prolonged exertion in the heat diverts blood flow to the body’s periphery (e.g., limbs) to help cool the body. This causes the wall of gut cells to break and open as less blood is surrounding the gut and providing the cells with the nutrients they need to stay tightly sealed.
Toxins and microbes can then move from the gut into the bloodstream, causing EIGS symptoms such as nausea, vomiting, diarrhoea, and possibly a full-body inflammatory response, or even death if left untreated.
Depending on the type, duration and environmental conditions, up to 85 per cent of endurance athletes, such as marathon runners, report experiencing these gut symptoms.
The study saw endurance-trained athletes run for two hours in 21.2-30.0°C and 35.0-37.2°C heat, with blood samples and temperatures taken at various points. It found that two hours of steady running (60 per cent of VO2max) in hot conditions could predict the magnitude of EIGS.
Ms Henningsen said while all parts of Australia were hot for part of the year, those working and playing sport in temperate climates such as Queensland, Northern Territory and Western Australia could be at even greater risk.
She and her team are now assessing nutrition strategies to maintain blood flow around the gut during exertional-heat stress, to help prevent gut damage. While strategies have been developed, such as carbohydrate and/or protein during exercise, consuming a high FODMAP diet and/or body cooling strategies, the new information will provide improved guidance.
“Findings from this research will not only help athletes’ performance and keep them safe, but will build upon Occupational Health, Safety and Environment practices within workplace settings to prevent adverse health outcomes to individuals who are exposed to prolonged exertional-heat stress,” Ms Henningsen said.