Hull York Medical School clinicians have identified a way of predicting early whether or not patients will develop a common type of Leukaemia, based on their genetics.
Dr David Allsup, Senior Lecturer at Hull York Medical School, University of Hull, and Haematology Consultant at Hull University Teaching Hospitals NHS Trust and Professor James Allan of Newcastle University, led the study that focused on the most common type of blood cancer: Chronic Lymphocytic Leukaemia (CLL).
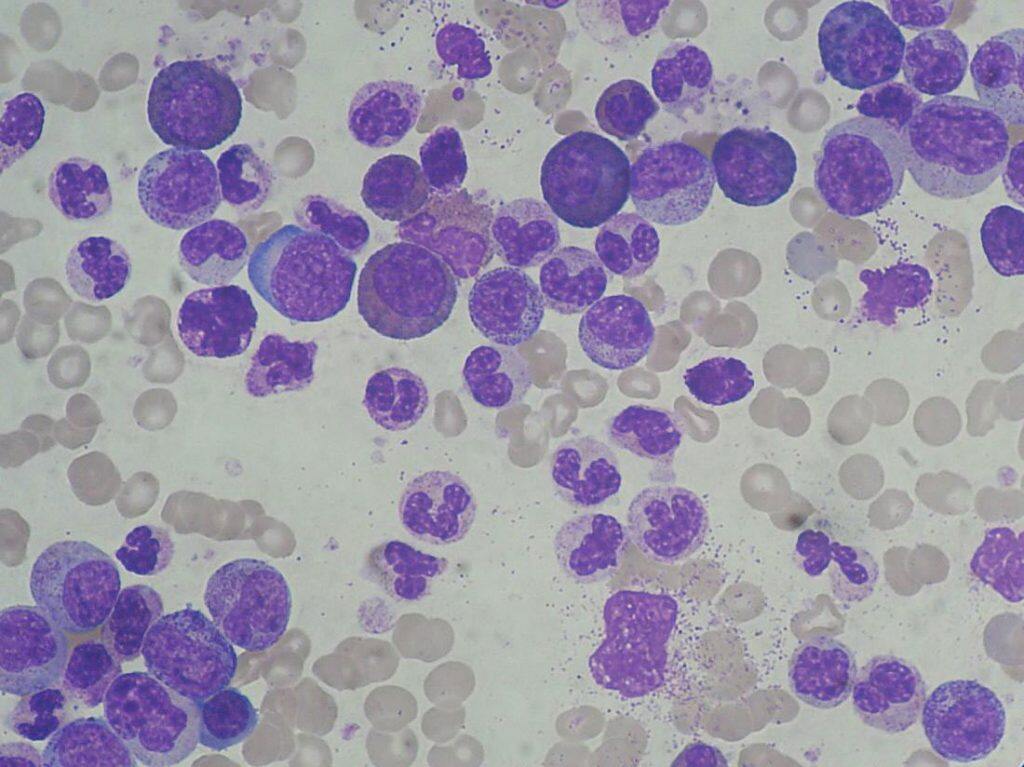
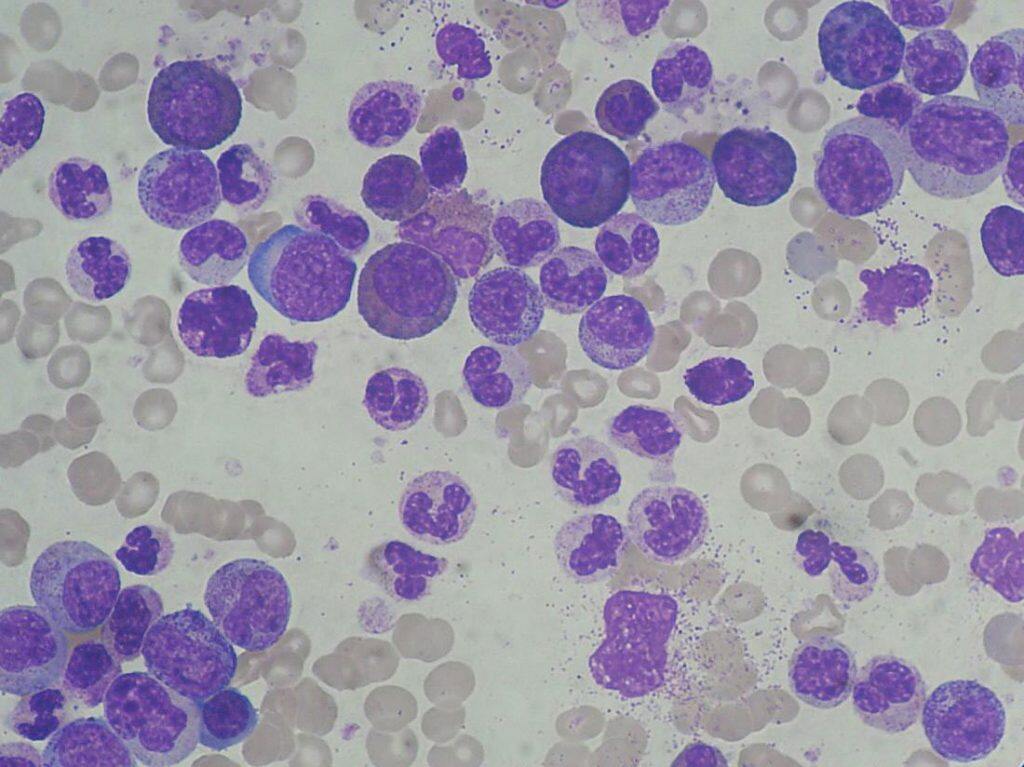
By examining blood samples of patients with CLL, Dr Allsup and Professor Allan discovered there was a genetic tendency to develop progressive forms of the illness in some patients.
Consequently, the study presents the opportunity in future to warn prospective patients that they also possess the genetic make-up that could lead to developing progressive CLL, and design a personalised treatment process for them long before the illness takes effect.
Dr Allsup said: “The study has demonstrated that CLL patients often possess the same genetic tendencies, and as such we can analyse the non-cancerous cells of prospective patients to predict the likelihood of future diagnosis.
“The study also allows us to move towards a more personalised diagnosis of leukaemia, and adapt our approach for patients based on the likelihood of them developing aggressive symptoms.”
CLL varies in its severity amongst patients; while some develop symptoms such as weight loss and lumps in the neck and armpits, others exhibit no symptoms at all, despite the leukaemia cells being present within their blood.
Dr Allsup said: “Not only does the research inform us if patients have the genetic tendency to develop progressive CLL, but it also enables us to determine whether or not a patient’s CLL will require treatment in the future or not.
“That way, we are able to keep a close eye on the patients with a high risk, and have treatment options available as soon as they are required.”
Professor Allan, from Newcastle University Centre for Cancer, said: “Emerging evidence suggests that early treatment for patients at high-risk of developing progressive CLL could significantly delay the onset of symptomatic Leukaemia and improve survival.
“The results from this collaborative study will help patients and their doctors make important decisions about when to start treatment.”
While this discovery does not constitute a cure for the disease, it goes a long way in identifying it in patients early, and thereby increasing their chances of survival.
Dr Allsup said: “On behalf of myself and my colleagues, we want to say a massive thank you to all of the volunteer patients that took part locally, without their cooperation in providing us with their blood samples, we wouldn’t have been able to conduct this research.”
As well as the patients that volunteered, Dr Allsup wanted to give recognition to Blood Cancer UK, Gilead Pharmaceuticals, Hull University Teaching Hospitals, and various local private benefactors, who all gave generous donations that allowed the research to be conducted.
The Daisy Tumour Bank also played a vital role in supporting the study: it housed blood samples that were examined for the research.
As a result of the discovery, the study has been published in the journal ‘Nature Communications’, one of the most highly cited multidisciplinary journals in the world.
Hull York Medical School is the joint medical school of the universities of Hull and York.
Professor Una Macleod, Dean of Hull York Medical School, said: “Hull York Medical School was founded on partnership and the desire to make a lasting difference to people’s lives. Across Hull and York our researchers are conducting world leading research to increase understanding and develop interventions for those conditions which most affect our communities. This research is an example of our commitment to making a difference and builds on our strong heritage of cancer research. I would like to congratulate Dr Allsup and Professor Allan for their work.”
The study was a collaborative effort between nine UK institutions, including Hull York Medical School, Newcastle University, Cardiff University, Leeds University, Leicester University, Liverpool University, Oxford University, Southampton University, and the Institute for Cancer Research in London.



































