Stem cells programmed to produce insulin in people with type 1 diabetes or to repair the heart muscle after a heart attack. Gene and cell therapies that improve cancer treatments. These new and innovative therapies have the potential to cure, alleviate and treat diseases where traditional medicines are currently insufficient.
The monk Gregor Mendel set more in motion than he could have imagined when, in the mid-19th century, he crossed yellow peas with green ones and thus began to map how traits are passed on to the next generation. Since then, research into how genes affect our traits, health and disease has grown to include entirely new forms of medicines.
Modern breakthroughs, such as the mapping of the human genome, the Nobel Prize-winning CRISPR gene editing scissors, the ability to rapidly map large amounts of DNA, and the Nobel Prize-winning discovery of how mature cells can be reprogrammed, have led to an increasing number of innovative biological therapies reaching patients.
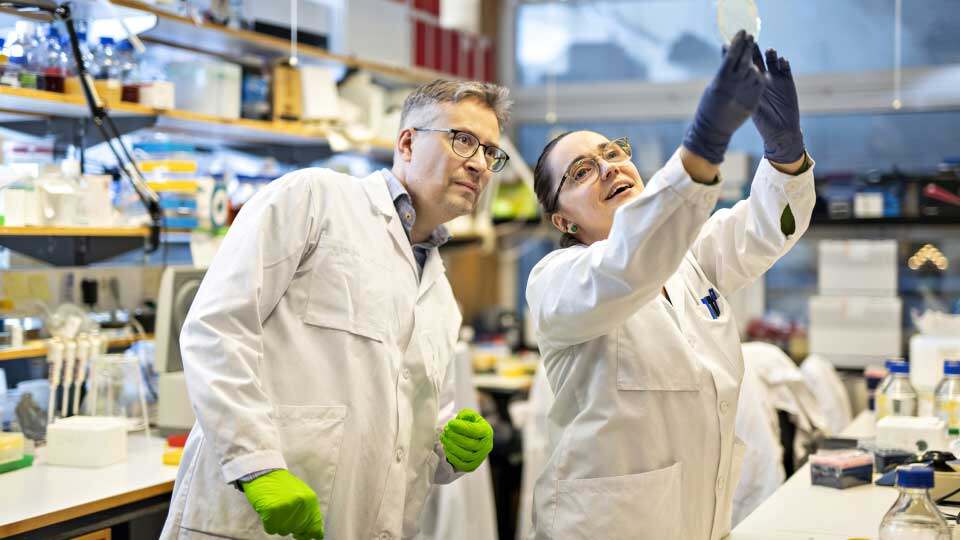
“These medicines differ from ‘ordinary’ medicines because the active substance is produced in or purified from materials of biological origin such as living cells, genes or tissue,” says Johan Flygare, researcher at the Lund Stem Cell Center and the Division of Molecular Medicine and Gene Therapy at Lund University.
These are therapies based on cells, genes or tissues and fall under the umbrella term ATMP (Advanced Therapy Medicinal Products).
“Advanced therapies are solving problems that previously could not be solved with traditional medicines. Instead of lifelong treatment of a disease caused by, for example, a defective gene, ATMP medicines have the potential to cure the patient by fixing the gene,” says Johan Flygare.
Healthy copy replaces faulty gene
Johan Flygare is researching a rare disease called Diamond-Blackfan anaemia, for which ATMP could play a major role. The disease is caused by a mutated gene that leads to a lack of the building blocks needed to form the cell’s protein factories (known as ribosomes).
“This in turn leads to the bone marrow not producing enough red blood cells, which means that the affected patient needs repeated blood transfusions,” says Johan Flygare.
Without a blood transfusion, the patient risks dying of anaemia. But regular transfusions carry a risk of iron poisoning, a side effect that can result in death. This is why Johan Flygare has been working as part of Stefan Karlsson’s research group to develop a curative gene therapy ever since he started his PhD at Lund University over 20 years ago.
“If we succeed, patients will be able to receive treatment that will allow their own blood stem cells to leave the bone marrow. We collect them and make sure to insert a healthy copy of the mutated gene into the cells which are then returned to the patient. We hope to start clinical trials in 2023,” says Johan Flygare.
“Tremendous joy in discovery”
Johan Flygare believes that there are many more rare diseases that could potentially be alleviated or cured by similar methods.
“One problem is that ATMPs are expensive to develop relative to the number of patients. It costs at least SEK 150 million to turn a lab discovery into a drug and conduct clinical trials. Despite 20 years of publishing over 20 scientific papers and clearly demonstrating that gene therapy has the potential to cure the disease, we were unable to find funding to bring the discovery to patients,” says Johan Flygare.
This changed two years ago when a private individual contacted them asking if they could help fund the project to clinical trials, which are crucial for the therapy to be approved and used to treat patients.
“Traditionally, pharmaceutical development is industry-driven, even though the discoveries may have been made in universities. However, almost all ATMPs originate from academic research and are developed in close collaboration with academia. That is unique. There is a tremendous feeling of joy in being able to set it up in the lab fairly quickly and see that there is potential there. But the next step is more complicated,” concludes Johan Flygare.
Different from traditional medicines
There are currently five approved ATMP treatments in Sweden, although more are on the way. Apart from the fact that treatments are expensive to develop, the regulatory framework and management processes have not kept pace with research, which is a challenge for the authorities responsible for approving clinical trials.
Now, many in the field are hoping that things will become clearer, and simpler, when the new Medicinal Products Act is negotiated next year (when Sweden holds the presidency of the Council of the EU for six months).
“Traditional medicines, like chemical substances, act more predictably in manufacturing or in a human body. Cell and gene therapies are much more complicated. That’s why the process becomes so important, from making the cells to treating the patient in the hospital,” says Elias Uhlin, project manager at the Lund Stem Cell Center.
Designed to help researchers
Elias Uhlin is currently building a pre-GMP centre in Lund that will help researchers develop their cell and gene therapies into treatments. GMP stands for Good Manufacturing Practice.
“In short, the process will move from treating rats in labs to treating patients in hospitals. This requires expertise in pharmaceutical development, knowledge of laws and regulations and access to advanced instruments. We hope to contribute with these things at the pre-GMP centre,” says Elias Uhlin.
Possible to grow heart cells
The Gene therapy field have progressed slightly further than cell therapies. But when scientists learned how to create cells that can develop into any cell type, called pluripotent stem cells, cell therapies enjoyed something of a renaissance.


“It is very concrete. You have a tiny cluster of cells, and by controlling development, two weeks later you have beating heart tissue, or a network of growing nerve cells. The research community cannot grow whole organs from stem cells at present, but it is possible to grow organ-specific cells, such as components of a heart. This gives researchers a whole new toolbox to develop treatments that could reach all kinds of patients,” says Elias Uhlin.



































